Special to the Philanthropy Journal
By Myechia Minter-Jordan, MD, MBA, Chief Impact Officer for DentaQuest
If you’re reading this, there is a good chance you have dental insurance, you brush your teeth, force yourself to floss and see the dentist on a (somewhat) regular basis, and make wryly sympathetic jokes when friends and colleagues do the same. Which means you have no personal experience with the problems I’m about to describe – problems that affect an astonishingly large number of Americans.
According to the National Association of Dental Plans, some 74 million Americans had no dental coverage in 2016, putting the dentally uninsured rate at nearly four times the rate for the medically uninsured. Forty three percent of rural Americans lack access to dental care, according to a National Rural Health Association report. And racial and socioeconomic disparities are exacerbated when it comes to oral health – 42 percent of adults with incomes below the federal poverty line have tooth decay, which is three times more than adults with higher incomes, says the Kaiser Commission on Medicaid and the Uninsured.
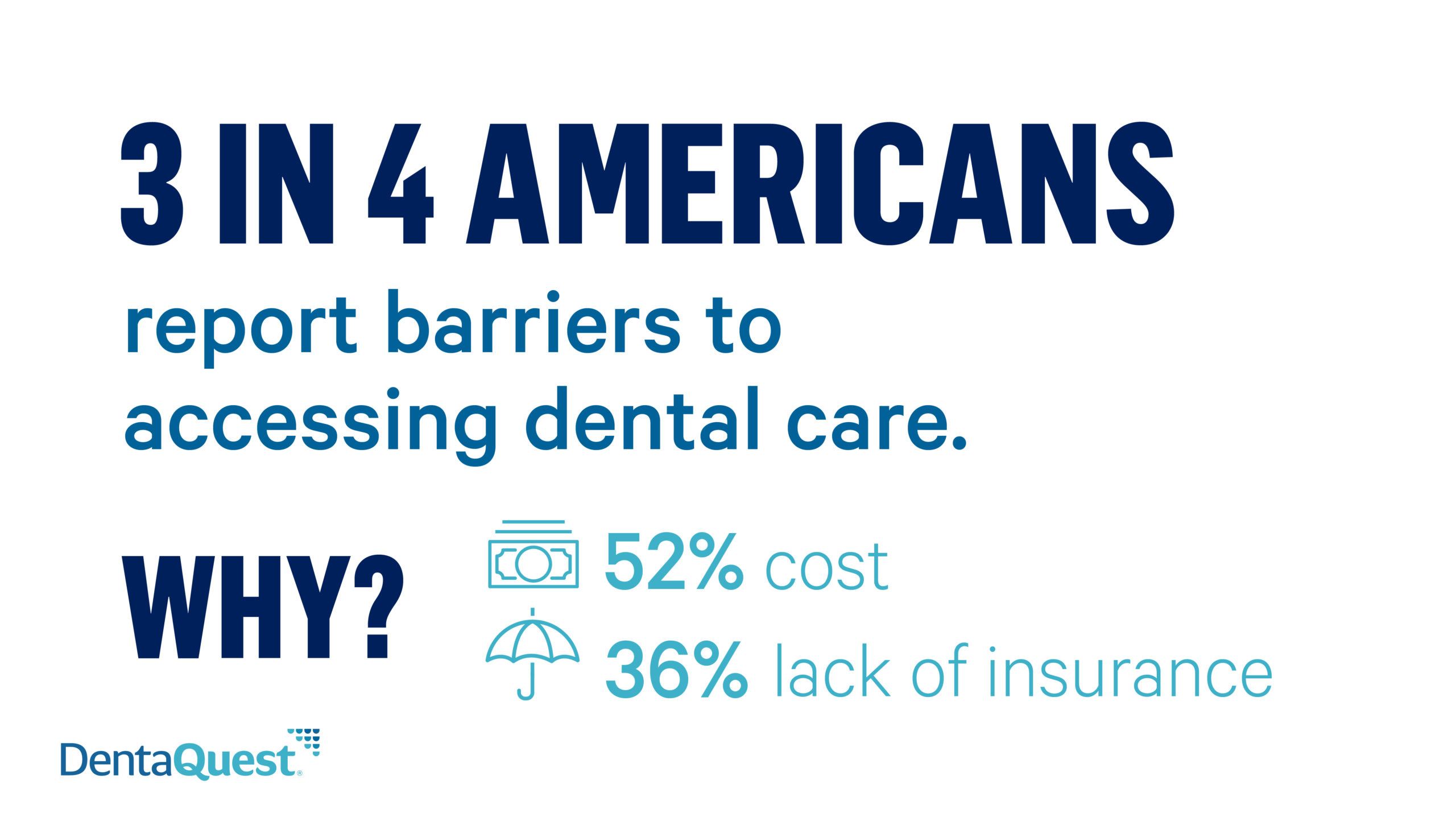
 These are problems that we at DentaQuest are dedicated to solving. We’re a double-bottom-line company with a mission to improve the oral health of all. The barriers to better care are indeed extensive and persistent; our own recently commissioned study – Reversible Decay: Oral Health is a Public Health Problem We Can Solve – dug deeper to understand why. But our study also found cause for hope: overwhelming agreement among patients, dentists, physicians, employers, and Medicaid dental administrators on a range of possible solutions – with prevention topping the list.
These are problems that we at DentaQuest are dedicated to solving. We’re a double-bottom-line company with a mission to improve the oral health of all. The barriers to better care are indeed extensive and persistent; our own recently commissioned study – Reversible Decay: Oral Health is a Public Health Problem We Can Solve – dug deeper to understand why. But our study also found cause for hope: overwhelming agreement among patients, dentists, physicians, employers, and Medicaid dental administrators on a range of possible solutions – with prevention topping the list.
Why is oral health so important? Because health starts in the mouth. And what’s at issue is about far more than who gets to sit in the dental chair and who does not – although that’s of course a big part of it. More broadly, poor oral health is linked to serious medical conditions such as heart disease, stroke, and diabetes. In fact, more than 90 percent of all systemic diseases have oral manifestations including swollen gums and mouth ulcers, and gum disease and oral infections impact the management and outcomes of systemic diseases and conditions. For example, diabetics with gum disease may have more problems maintaining their blood glucose at recommended levels. And, according to a report in the Journal of Neurology, Neurosurgery & Psychiatry, adults with gingivitis performed worse on tests of memory and other cognitive skills than did those with healthier mouths. But the negative ripple effect doesn’t stop there. Children who have poor oral health often miss more school and receive lower grades than children who don’t, as the Centers for Disease Control (CDC) has noted. And each year, more than $6 billion is lost in productivity due to people missing work for dental issues.
 Yet for too long, we have viewed the way we receive and pay for oral care as being completely separate from the way we prevent and treat our overall health needs. Like behavioral health before it, oral health has been neglected and siloed from the rest of the healthcare ecosystem.
Yet for too long, we have viewed the way we receive and pay for oral care as being completely separate from the way we prevent and treat our overall health needs. Like behavioral health before it, oral health has been neglected and siloed from the rest of the healthcare ecosystem.
To that end, outdated payer and dental care delivery models need to catch up with the promising changes being made in primary care and the related shift from fee-for-service to value-based care. Oral health has been left out of recent national initiatives to change our health insurance system like the Affordable Care Act (ACA) and reforms to Medicare. It’s too often an afterthought, despite the significant potential cost savings that could be achieved with changes. A September 2018 bipartisan letter from 28 US senators urging dental coverage be made available to Medicare recipients suggested this could generate savings of $63.5 billion over 10 years.
It’s likely that healthcare, on a policy level, will be an area of increased focus over the next several years – and it’s imperative that oral health be part of that conversation, not as an afterthought but as an integral component.
Fueling an oral health transformation: social investment and strategic partnerships
As the policy discussions unfold, foundations and funders meanwhile have an opportunity to play a larger role in supporting nonprofits and research organizations working to improve oral health outcomes – and in that process, shape the debate. The DentaQuest Partnership for Oral Health Advancement is working to address what we know to be underinvested areas of oral health that are critical to providing better care to more people.
Since 2009, we have provided more than $200 million in funding for research, care improvement initiatives and grants to improve oral health. Our investments in hundreds of organizations across all 50 states has helped improve oral health for many.
As a leader and key funder in the creation of the Oral Health 2020 Network, now the Oral Health Progress and Equity Network (OPEN), DentaQuest has been fortunate to be a part of a growing national network of individuals and organizations that believe oral health is essential to overall health and wellbeing. The OPEN Network has made significant progress toward many of its initial goals, such as a reduction in caries experience in very young children and movement towards an extensive dental benefit in Medicare, but systemic problems still exist, and the work must continue.
A call to action for better oral health
As we look to the future and evolve our grant making strategy, at DentaQuest we are increasing our commitment in areas where we believe our organizational strengths and expertise are especially well suited to help meet the challenge:
- A single, national oral health measurement system. We must have complete and consistent data on oral health status to make sure everyone is measured by the same standards. With a unified system, we’ll be better able to target resources and interventions, and to measure progress. If you can’t measure it, you can’t fix it.
- A public adult dental benefit is needed to expand access to adults. Since children’s dental benefits are mandatory in Medicaid, most Medicaid eligible children have access to dental benefits through Medicaid. For low-income adults, however, the provision of Medicaid dental coverage is an optional benefit and varies widely across states. Some provide coverage for emergency procedures only; others provide no coverage at all. And Medicare, with just a few exceptions, doesn’t provide coverage either, as most adults are unhappily surprised to learn. So the preventative care that is so critical to better oral – and overall – health goes missing.
- Person-centered care that will transform the oral health industry. This includes both a value-based care model and interprofessional practice. While the value-based care model is advancing in primary healthcare, it’s struggling to get traction in oral health. We need to change the way dentists and other providers are reimbursed with a focus on quality outcomes, not the volume of care provided. We must also make it easier for multiple caregivers to work collaboratively, within and across settings, to improve the quality of care. By putting people at the center, we will strengthen the system and ensure quality care for more people at a lower cost.
While these are the areas where the DentaQuest Partnership will focus its resources and energy, more engagement and investment is needed in other critical areas of oral health. Even as more like-minded parties come to see that oral health is not just part of the healthcare ecosystem, but a critical piece of a broken system that needs to be fixed, developing and implementing those fixes will require broad participation. If you are passionate about our children’s education, oral health matters to you. If you believe that the nation that spends the most on healthcare isn’t nearly as healthy as it should be, oral health matters to you. If you understand that positive changes can be made – today – then oral health matters to you.
Together, by making strategic investments in oral health with the larger healthcare community, we can improve oral health and overall wellness – not just for some, but for all.
Dr. Myechia Minter-Jordan is Executive Vice President and Chief Impact Officer for DentaQuest. In this role she oversees the DentaQuest Partnership for Oral Health Advancement (the Partnership) and Impact Group, leading research and grantmaking activities focused on improving oral health, integrating oral health and overall health through medical/dental collaborations, moving toward a value-based payment model, and guiding a growing research and data portfolio.
Dr. Jordan joined DentaQuest after six years at the Dimock Center, in Roxbury Massachusetts. Considered a national model for comprehensive health and human services, Dimock focuses on the integration of clinical and behavioral health, treats more than 19,000 people annually through its comprehensive programs, and is and the second largest health center in the Boston area. As Chief Medical Officer, she was responsible for successfully transitioning to an Electronic Medical Record system, established Dimock’s first Institutional Review Board, and led the 2012 effort to receive a $4.9 million federal Health Resource Services Administration (HRSA) grant that expanded and transformed Dimock from a health center facility to a primary medical home.
As CEO, Dr. Jordan played a leadership role in developing the Harvard Primary Care Center Initiative that partners academic hospitals and community health centers to transform them into patient centered medical homes. Through her work with the Harvard Catalyst Clinical and Translational Science Center, she also created an infrastructure for clinical research at Dimock, which will ensure that patients are meaningfully engaged in the creation and approval of research initiatives. Dr. Jordan formed partnerships linking Dimock to world-class institutions, including The Harvard Medical School, Beth Israel Deaconess Medical Center and Partners HealthCare.
Dr. Jordan graduated from Brown University School of Medicine, and the Johns Hopkins University Carey School of Business. She worked for Johns Hopkins Medicine as an attending physician and instructor of medicine and then served as the Director of Medical Consultation Services at Johns Hopkins Bayview Medical Center. She also received an honorary Doctor of Public Service degree from Northeastern University and an honorary Doctor of Humane Letters degree from Newbury College.
In 2015, she was appointed to the Commonwealth of Massachusetts Health Planning Council Advisory Committee and the Boston Public Health Commission. In 2018, she was appointed as Vice-Chair of the Board of the RIZE Fund, a statewide collaborative of substance use treatment providers, legislative leaders and funders, that promotes and expands strong models to combat the opioid epidemic. She also serves on the Boards of the Isabella Stewart Gardner Museum, Yawkey Foundations, Harvard Pilgrim Health Care and The Boston Foundation.
Dr. Jordan lives in West Roxbury with her husband and two daughters.